How Doctors Diagnose Hernias: Scans, Tests & Clinical Exams
Several factors lead to the development of hernias, which include aging, regular wear and tear, a scar left from previous surgery, or they might be due to birth defects or genetic disorders. Some of the most common areas in which hernias may occur are the lower chest, groin, line of the abdomen, or near the incision of previous abdominal surgery.
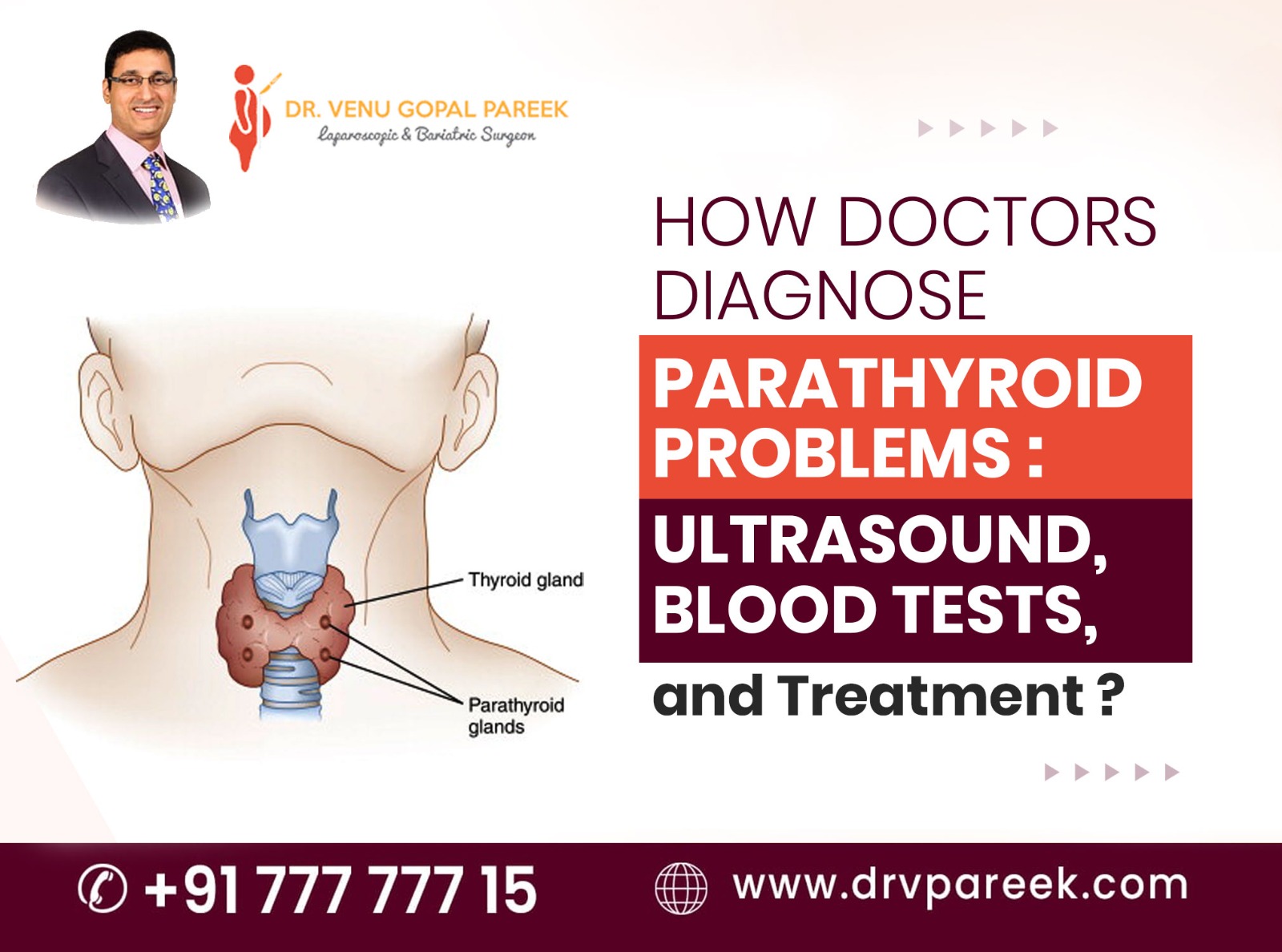
How are hernias diagnosed?
Sometimes it hart to detect a hernia, especially in its early stages. The bulge can be visible in some cases, but in other cases it shows up and then disappears. When it disappears, it doesn’t mean the hernia has healed itself; instead, the content in the hernia sac just goes back through the same weak spot they pushed out in the abdominal wall—the weak spot stays until you get a surgical repair.
Hernias can be actually diagnosed by
- Physical Examination
- X-Ray
- Endoscopy
- Ultrasound
- CT scan of abdomen
- MRI scan of the abdomen
However, the most direct approach is a physical examination by a surgeon who has good experience in hernia repairs.
A diagnostic scan might reveal that there are bulges in the abdominal wall, but they cannot always distinguish the size of the hernia. Sometimes it may fail to differentiate whether the bulge is a hernia or a natural fold of the abdominal wall. In many patients the imaging indicated the presence of a hernia during their first diagnosis; later it was proven that no hernia was clinically present.
In such cases, it may be wiser to wait and see if the hernia develops over time rather than going for an unnecessary hernia repair surgery.
Also, not finding a hernia in a diagnostic image doesn’t mean there is no hernia. Dr. Venugopal Pareek, one of the best hernia surgeons, says that on some occasions the imaging tests have not shown any signs of hernia, but upon physical examination, a hernia was found.
Advanced clinical techniques to diagnose Hernias
During a physical examination, surgeons does not simply check for a bulge; they perform various procedures to increase intra-abdominal pressure—although the majority of people know about the “cough test,” doctors often prefer the Valsalva technique (taking a deep breath and forcefully exhaling by closing the mouth and nose). This technique creates an internal pressure that lasts for a few seconds rather than a short pressure spike in the cough test. This technique can help to discover even a small defect, which otherwise may not be visible.
Another important factor is the patient’s position. Doctors examine the patient thoroughly in various positions when they lie down, stand up, and bend. In the lying-down position, a surgeon might clearly feel the muscle defect edges, whereas, in the standing position, the hernia contents protrude due to gravity, thus making the diagnosis more apparent.
Dynamic ultrasound vs. static scans
The next choice of diagnosis is ultrasound, especially when the physical examination fails to confirm hernia. The procedure involves the patient lying still on a table, and the doctor uses a transducer (or probe), which emits high-frequency sound waves, to see your tissues moving as you cough or strain in real time. This real-time procedure is one of the best methods for detecting tiny hernias that only become visible under stress.
Occult hernias—many of you have not heard about this term, which refers to a situation when a patient is experiencing persistent pain but a bulge cannot be felt. Even the CT scans, which are outstanding in case of emergencies because of their rapidity and 94% sensitivity rate, sometimes fail to detect these “hidden” defects. In such circumstances, an MRI is considered the most reliable test. Since MRI provides better soft-tissue contrast, studies have demonstrated that it can identify occult hernias correctly in more than 91% of instances where a CT scan was negative.
In the case of internal hernias (e.g., hiatal), surgeons generally perform an upper GI endoscopy (EGD) to detect certain anatomical defects.
Impact of late diagnosis
If a diagnosis is delayed, the patient may end up with complications that are not only life-threatening but also difficult to treat. A hernia becomes incarcerated when the tissue that has herniated (popped out) gets trapped and cannot be forced back in. This may further result in strangulation—the blood supply to this portion of the herniated organ is restricted. This is an emergency condition where the surgeon has to act soon because the tissue may start to die within 4 hours.
Symptoms indicating emergency:
- Unexpected occurrence of excruciating pain that intensifies very fast.
- The swelling changes its color to red, purple, or black.
- Vomiting, nausea, and fever.
- Unable to pass gas or have a bowel movement.
In these emergency situations, doctors usually observe the elevated levels of white blood cell counts or C-reactive protein (CRP); both of them indicate the tissue that is trapped is at risk. Early diagnosis through a proper clinical examination is the fastest and most effective way to detect and treat these conditions at an early stage.